 Alzheimer’s and Dementia Care… The road ahead
Alzheimer’s and Dementia Care… The road ahead
Caring for a loved one with Alzheimer’s disease and other types of dementia can be a challenge, not only for the person diagnosed but also for their spouses and family members. Although caring for someone with Alzheimer’s or dementia can seem overwhelming at times, the more information & support you have, the better you will handle the demands and determine the long-term care options that are best suited to you and your loved one.
THIS ARTICLE WILL DEAL WITH:
- Preparing yourself for the care
- Developing routines
- Engaging your loved one in activities
- Planning activities with your loved one
- Handling challenges as they present themselves
- Considering long term care
- Assessing assisted living or nursing homes
Preparing yourself for Alzheimer’s & dementia care
You may be dealing with a whole range of emotions and concerns, as you come to grips with an Alzheimer’s or other dementia diagnosis. There’s no doubt you will be worried about how your loved one will change, how you will keep him or her safe & comfortable, and how much your life will change in order to sustain it. Emotions such as anger, grief, and shock will be likely to be experienced. Adjusting to this new reality is neither, easy or immediate. It is critically important to give yourself some time, process the road ahead and reach out for help and support from a number of resources available. The more support you have, the better you will be able to help and manage your loved one, care.
While some of these tips are aimed specifically for people with Alzheimer’s, they can equally apply to persons suffering with other types of dementia.
Early-stage Alzheimer’s care preparations
Some Alzheimer’s & Dementia care preparations that are best done sooner rather than later. It’s hard to consider these questions at first, as it means thinking about a time when you or your loved one is already well down the road of his or her Alzheimer’s journey. However, putting such preparations in place early helps a smoother transition for everyone later on. Depending on the stage of diagnosis, include the person with Alzheimer’s & Dementia in the decision-making process as much as possible. If the person is at a more advanced stage of dementia, at least try to act on what their wishes would be.
Questions to consider in preparing for Alzheimer’s and dementia care:
▪ Who will make healthcare and financial decisions when the person is no longer able to do so?
While this is difficult topic to raise, if your loved one is still lucid enough, getting their wishes down on paper means they’ll be preserved and respected by all members of the family. Consider having a family meeting involving the person and those who may be impacted with the decisions being made (all children, and or grandchildren who may have to ultimately step up and take on a role in their care). In most cases such family meetings can go smoothly as it pertains to respecting the affected person’s wish. However, do not hesitate to involve an elder law attorney to best understand your options. You’ll need to consider power of attorney, both for finances and for healthcare. If the person has already lost capacity, you may need to apply for guardianship/conservatorship. Last but not least, their Personal Will if one is not in place already.
▪ How will care needs be met?
It is not uncommon that some family members assume that a spouse or nearest family member can take on the role of caregiver, but this assumption is not always the case or even possible. Caregiving is a rather a large commitment, and one that becomes greater over time. The person with Alzheimer’s and or advanced Dementia will eventually need round-the-clock personal care. Although family members are more than willing to take this challenge on, many family members may have their own health issues, jobs, and other roles & responsibilities. Communication is essential to ensure that the needs of the affected person are known & met, and that the caregiver has all the support in place to meet those needs.
▪ Where will the person live?
Knowing their wishes ahead of time will certainly ease the process in making this decision. Their own home will more than likely be their first wish. However, before concluding that home care is the final decision, consider a home assessment to determine the appropriateness of the home to meet their care needs. An assessment can be performed free of cost and determine the care needs and client’s challenges for today and moving forward. This way you will know if perhaps the home is fine for now, but difficult to access or make safe for later. On the other hand, the home could be fully suitable for their care… now and to meet future challenges. This is the type of information that will be invaluable to make informed decisions. If the person is currently living alone, for example, or far from any family, it may be necessary to relocate or consider care options that best suits their need, care, wishes… or a facility with more support.
Find out what assistance your medical team can provide in these areas. In some countries, you can also hire a care manager privately. Geriatric care managers can provide an initial assessment as well as assistance with managing your case, including crisis management, interviewing in-home help, or assisting with placement in an assisted living facility or nursing home.
Developing day-to-day routines
Having a daily routine in Alzheimer’s & Dementia care helps caregiving run smoothly. These routines won’t be set in stone, but they give a sense of consistency, which is beneficial to the Alzheimer’s patient even if they can’t communicate it.
While every family will have their own unique routine, you can get some great ideas from your medical team or Alzheimer’s support group, especially regarding establishing routines to handle the most challenging times of day, such as evenings.
- Keep a sense of structure and familiarity. Try to keep consistent daily times for activities such as waking up, mealtimes, bathing, dressing, receiving visitors, and bedtime. Keeping these things at the same time and place can help orientate the person.
- Let the person know what to expect even if you are not sure that he or she completely understands. You can use cues to establish the different times of day. For example, in the morning you can open the curtains to let sunlight in. In the evening, you can put on quiet music to indicate it’s bedtime.
- Involve the person in daily activities as much as they are able. For example, a person may not be able to tie their shoes, but may be able to put clothes in the hamper. Clipping plants outside may not be safe, but the person may be able to weed, plant, or water. Use your best judgment as to what is safe and what the person can handle.
Communication tips
As your loved one’s Alzheimer’s progresses, you will notice changes in communication. Trouble finding words, increased hand gestures, easy confusion, even inappropriate outbursts are all normal. Here are some tips, do’s and don’ts on communicating:
| Communication Do’s and Don’ts? |
| Do |
| Avoid becoming frustrated by empathizing and remembering the person can’t help their condition. Making the person feel safe rather than stressed will make communication easier. Take a short break if you feel your fuse getting short. |
| Keep communication short, simple and clear. Give one direction or ask one question at a time. |
| Tell the person who you are if there appears to be any doubt. |
| Call the person by name. |
| Speak slowly. The person may take longer to process what’s being said. |
| Use closed-ended questions, which can be answered as “yes” or “no.” For example, ask, “Did you enjoy the beef at dinner?” instead of “What did you have for dinner?” |
| Find a different way to say the same thing if it wasn’t understood.Try a simpler statement with fewer words. |
| Use distraction or fibs if telling the whole truth will upset the person with dementia. For example, to answer the question, “Where is my mother?” it may be better to say, “She’s not here right now” instead of “She died 20 years ago.” |
| Use repetition as much as necessary. We prepared to say the same things over and over as the person can’t recall them for more than a few minutes at a time. |
| Use techniques to attract and maintain the person’s attention. Smile, and make eye contact, use gestures, touch, and other body language. |
| Don’t |
| Ever say things like: “Do you remember?” “Try to remember!” “Did you forget?” “How could you not know that?!” |
| Ask questions that challenge short-term memory, such as “Do you remember what we did last night?” The answer will likely be “no,” which may be humiliating for the person with dementia. |
| Talk in paragraphs. Instead, offer one idea at a time. |
| Point out the person’s memory difficulty. Avoid remarks such as “I just told you that.” Instead, just repeat it over and over. |
| Talk in front of the person as if he or she were not present. Always include the person in any conversation when they are physically present. |
| Use lots of pronouns such as “there, that, those, him, her, it.” Use nouns instead. For example, instead of “sit there” say “sit in the blue chair.” |
| Use slang or unfamiliar words. The person may not understand the latest terms or phrases. |
| Use patronizing language or “baby talk”. A person with dementia will feel angry or hurt at being talked down to. |
| Use sarcasm or irony, even if meant humorously. Again, it can cause hurt or confusion. |
Planning activities and visitors
As you develop daily routines, it’s important to include activities and visitors into their life. You want to make sure that the Alzheimer’s patient is getting sensory experiences and socialization, but not to the point of getting over-stimulated and stressed. Here are some suggestions for activities:
- Start with the person’s interests.
- Ask family and friends for memories of interests the person used to have. You’ll want to tailor the interests to the current level of ability so the person doesn’t get frustrated.
- Vary activities to stimulate different senses of sight, smell, hearing, and touch. For example, you can try singing songs, telling stories, movement such as dance, walking, or swimming, tactile activities such as painting, working with clay, gardening, or interacting with pets.
- Planning time outdoors can be very therapeutic. You can go for a drive, visit a park, or take a short walk. Even sitting on a balcony or in the backyard can be relaxing.
- Consider outside group activities designed for those with Alzheimer’s. Senior centers or community centers may host these types of activities. You can also look into adult day care programs, which are partial or full days at a facility catering to older adults and/or dementia patients.
Visitors and social events
Visitors can be a rich part of the day for a person with Alzheimer’s disease. It can also provide an opportunity for you as the caregiver to socialize or take a break. Plan visitors at a time of day when your loved one can best handle them. Brief visitors on communication tips if they are uncertain and suggest they bring memorabilia your loved one may like, such as a favorite old song or book. Family and social events may also be appropriate, as long as the Alzheimer’s patient is comfortable. Focus on events that won’t overwhelm the person; excessive activity or stimulation at the wrong time of day might be too much to handle.
Handling challenges in Alzheimer’s and dementia care
One of the painful parts of Alzheimer’s disease is watching your loved one, display behaviours you never would have thought possible. Alzheimer’s can cause substantial changes in how a person acts. This can range from the embarrassing, such as inappropriate outbursts, to wandering, hallucinations, and even violent behaviour. Everyday tasks like eating, bathing, and dressing can become major challenges.
As painful as some behaviours are, it’s critical not to blame yourself or try to handle all the changes in behaviour alone. As the challenging behaviour progresses, you may find yourself too embarrassed to go out, for example, or to seek respite care. Unfortunately, difficult behaviour is part and parcel of Alzheimer’s disease. Don’t isolate yourself. Ask for help from the medical team and reach out to caregiver groups for support. There are ways to modify or better accommodate problem behaviours. Both the environment you create at home and the way you communicate with your loved one can make a substantial difference.
Considering long-term Alzheimer’s and dementia care
It’s the nature of Alzheimer’s disease to progressively get worse as memory deteriorates. In the advanced stages of Alzheimer’s, your loved one will likely need round-the-clock care. Thinking ahead to these possibilities can help make decisions easier.
Care at home
There are several options for extending care at home:
- In-home help refers to caregivers that you can hire to provide assistance for your loved one. In-home help ranges from a few hours a week of assistance to live-in help, depending on your needs. You’ll want to evaluate what sort of tasks you’d like help with, how much you can afford to spend, and what hours you need. Getting help with basic tasks like housekeeping, shopping, or other errands can also help you provide more focused care for your loved one. Be sure to look for a service provider who has extensive Geriatric Care experience.
- Day programs, also called adult day care, are programs that typically operate weekdays and offer a variety of activities and socialization opportunities. They also provide the chance for you as the caregiver to continue working or attend to other needs. There are some programs that specialize in dementia care. Alternatively, you can hire a caregiver for the days you need it for without any time commitment. This may alleviate some stress on the part of the patient, as they do not have to leave their familiar surroundings.
- Respite care. Respite care is short-term care where your loved one stays in a facility temporarily. This gives you a block of time to rest, travel, or attend to other things. Of course, you can hire a caregiver for the block of time desired. This may alleviate some stress on the part of the patient, as they do not have to leave their familiar surroundings.
Is it time to move?
As Alzheimer’s progresses, the physical and mental demands on you as caregiver can gradually become overwhelming. Each day can bring new additional challenges. The patient may require total assistance with physical tasks like bathing, dressing, and toileting, as well as greater overall supervision. At some point, you won’t be able to leave your loved one alone. Nighttime behaviours may not allow you to sleep, and with some patients, belligerent or aggressive behaviours may exceed your ability to cope or feel safe. Every situation is different. Sometimes, you can bridge the gap by bringing in additional assistance, such as in-home help or other family members to share the caregiving burden. However, it is not a sign of weakness if moving to your loved one to a facility seems like the best plan of care. It’s never an easy decision to make, but when you’re overwhelmed by stress and fatigue, it’s difficult to maintain your caregiving standards. If the person with Alzheimer’s is living alone, or you as the primary caregiver have health problems, this option may need to be considered sooner rather than later.
When considering your caregiving options, it’s important to consider whether you are able to balance your other obligations, either financial or to other family members. Will you be able to afford appropriate in-home coverage if you can’t continue caregiving? Talk to your loved one’s medical care team for their perspective as well.
Evaluating an assisted living facility or nursing home
If the best choice is to move the Alzheimer’s patient to a facility, it doesn’t mean you will no longer be involved in their care. You can still visit regularly and ensure your loved one gets the care he or she needs. Even if you are not yet ready to make that step, doing some initial legwork might save a lot of heartache in the case of a crisis where you have to move quickly. The first step is finding the right place for your loved one.
Choosing a facility
There are two main types of facilities that you will most likely have to evaluate for a loved one with Alzheimer’s: an assisted living facility or a nursing home.
Assisted Living
Assisted living is an option for those who need help with some activities of daily living. Some facilities provide minor help with medications as well. Staff are available twenty-four hours a day, but you will want to make sure they have experience handling residents with Alzheimer’s disease. Also be clear about what stage your loved one is at, as he / she may need to move to a higher level of care.
Nursing Home
Nursing homes provide assistance in both activities of daily living and a high level of medical care. A licensed physician supervises each resident’s care and a nurse or other medical professional is almost always on the premises. Skilled nursing care providers and medical professionals such as occupational or physical therapists are also available.
How do I choose a facility?
Once you’ve determined the appropriate level of care, you’ll want to visit the facility announced and unannounced—to meet with the staff and otherwise evaluate the home. You will also want to evaluate the facility based on their experience with Alzheimer’s residents. Facilities that cater specifically for Alzheimer’s patients should have a designated area, for residents with dementia.
Questions to ask such a facility include:
- Policy and procedures – Does the unit mix Alzheimer’s patients with those with mental illness, which can be dangerous? Does the program require the family to supply a detailed social history of the resident (a good sign)?
- Environment – Is the unit clean? Is the dining area large enough for all residents to use it comfortably? Are the doors alarmed or on a delayed opening system to prevent wandering? Is the unit too noisy?
- Staffing – What is the ratio of residents to staff? (5 to 1 during the day, 9 to 1 at night is normal). What is staff turnover like? How do they handle meals and ensure adequate hydration, since the person can often forget to eat or drink? How do they assess unexpressed pain—if the Alzheimer’s resident has pain but cannot communicate it?
- Staff training – What training for Alzheimer’s care do they have? Does the facility provide staff with monthly in-service training on Alzheimer’s care?
- Activities – Is there an activity plan for each resident based on the person’s interests and remaining cognitive strengths? Are residents escorted outside on a daily basis? Are regular outings planned for residents?
- Services – Does the unit provide hospice services? What were the findings in the most recent Ministry conducted inspection? What are the rates of infectious outbreaks? What is the resident rate of injury incidences?
What to expect during a transition
Moving is a big adjustment both for the person with Alzheimer’s and you as their caregiver. Your loved one is moving to a new home environment with new faces and places. You are adjusting from being the person providing hands-on care to being an advocate. Remember to give yourself and the Alzheimer’s patient time to adjust. If you’re expecting to move, try to have essentials packed and ready to go, and as many administrative details taken care of as possible, as sometimes beds can come up quickly. Work closely with staff regarding your loved one’s needs and preferences. An extra familiar face during moving day, such as another relative or close friend, can also help.
Each person adjusts differently to this transition. Depending on your loved one’s needs, you may either need to visit more frequently or give your loved one their own space to adjust. As the adjustment period eases, you can settle into the visiting pattern that is best for both of you.
Please contact us today, to discuss any challenges you may be facing and how our services can help you remain independent, protected, safe, and in you home / community.
You got questions, we have answers: (905) 785-2341 or email us at


 Talking about the future can be hard. Such discussion will invoke anxiety in even the most calm of us when we start to think about all the unknowns in our futures and those of our loved ones. These discussions can get even harder when it’s not our future we’re talking about, but rather someone else’s. However, as difficult as it may be, there are some questions that we need to have answers to when it comes to our ageing parents and it is wise to have these conversations sooner rather than later. On that note, here are 7 basic questions that you should include in the “talk” with your ageing parent/s… as soon as you can.
Talking about the future can be hard. Such discussion will invoke anxiety in even the most calm of us when we start to think about all the unknowns in our futures and those of our loved ones. These discussions can get even harder when it’s not our future we’re talking about, but rather someone else’s. However, as difficult as it may be, there are some questions that we need to have answers to when it comes to our ageing parents and it is wise to have these conversations sooner rather than later. On that note, here are 7 basic questions that you should include in the “talk” with your ageing parent/s… as soon as you can. Sometimes there’s a lot of pressure to do things in a “traditional” way when it comes to how we remember our loved ones, but that’s not always what they want. Although funerals/memorials need to reflect both the person that is gone and those who are left behind, having a discussion ahead of time can mean that all sides get their voices heard. When a decision is reached beforehand, our loved ones know their wishes will be respected and those of us left behind can know we’re memorializing our parents in a way that they accept as well. This means no guilt for anyone and that’s a much-needed relief at a time of sorrow.
Sometimes there’s a lot of pressure to do things in a “traditional” way when it comes to how we remember our loved ones, but that’s not always what they want. Although funerals/memorials need to reflect both the person that is gone and those who are left behind, having a discussion ahead of time can mean that all sides get their voices heard. When a decision is reached beforehand, our loved ones know their wishes will be respected and those of us left behind can know we’re memorializing our parents in a way that they accept as well. This means no guilt for anyone and that’s a much-needed relief at a time of sorrow.
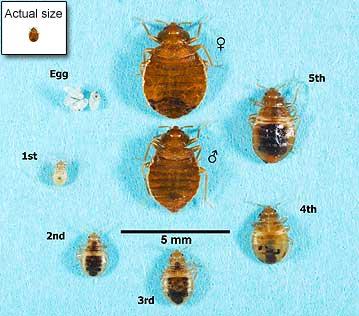 Bedbugs are small, oval, brownish insects that live on the blood of animals or humans. Adult bedbugs have flat bodies about the size of an apple seed. After feeding, however, their bodies swell and are a reddish color.
Bedbugs are small, oval, brownish insects that live on the blood of animals or humans. Adult bedbugs have flat bodies about the size of an apple seed. After feeding, however, their bodies swell and are a reddish color.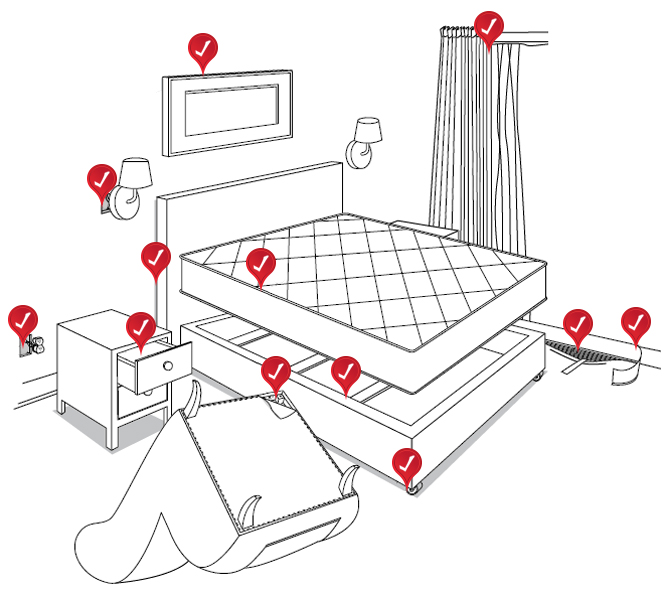 Bedbugs may enter your home undetected through luggage, clothing, used beds, couches and other items.
Bedbugs may enter your home undetected through luggage, clothing, used beds, couches and other items. Bedbugs are active mainly at night and usually bite people while they are sleeping. They feed by piercing the skin and withdrawing blood through an elongated beak. The bugs feed from three to 10 minutes to become engorged and then crawl away unnoticed.
Bedbugs are active mainly at night and usually bite people while they are sleeping. They feed by piercing the skin and withdrawing blood through an elongated beak. The bugs feed from three to 10 minutes to become engorged and then crawl away unnoticed.


 Alzheimer’s was first identified by Alois Alzheimer in 1906 in Germany and is the most common type of dementia, a general term for impaired brain functioning. Other dementias include
Alzheimer’s was first identified by Alois Alzheimer in 1906 in Germany and is the most common type of dementia, a general term for impaired brain functioning. Other dementias include
